Introduction:
Since the 1950s niacin (vitamin B3) has been known to be effective in lowering blood cholesterol levels. In the 1970s the famed Coronary Drug Project demonstrated that niacin was the only cholesterol-lowering agent to actually reduce overall mortality. Niacin typically lowers LDL levels by 16–23% while raising HDL levels by 20–33%. These effects, especially the effect on HDL, compare quite favorably with conventional cholesterol-lowering drugs (i.e., statin drugs like Crestor, Lipitor, Zocor, etc.).
Niacin has also been shown to lower the more harmful Lp(a) lipoprotein, triglycerides, and lower markers of inflammation such as CRP and fibrinogen
Background Information:
Several studies have compared niacin with standard lipid-lowering drugs, including statins. These studies have shown significant advantages for niacin. While statins produce a greater LDL reduction, niacin provides better overall results as the percentage increase in protective HDL is dramatically in favor of niacin. Niacin also is very useful in patients with the more damaging small and dense form of LDL particle or lipoprotein(a). Here is a table from a study comparing niacin to Lipitor.
|
Atorvastatin |
Niacin |
|||
| Parameter | Before | After | Before | After |
| Total LDL (mg/dl) |
110 |
56 |
111 |
89 |
| LDL peak diameter |
251 |
256 |
253 |
263 |
| Lipoprotein(a) (mg/dl) |
45 |
44 |
37 |
23 |
| HDL (mg/dl) |
42 |
43 |
38 |
54 |
While niacin exerts significant benefit on its own, it does not appear to enhance the benefits of statins in well-controlled patients (LDL levels below 100 mg/dl). The AIM-HIGH study funded by the National Heart, Lung, and Blood Institute recruited 3,400 patients who were at risk for heart trouble despite the fact that their LDL was under control with the use of a statin drug (simvastatin [Zocor]) these patients were given niacin to see if there was an additive effect. The study ended 18 months early because no additional cardiovascular benefit was seen in those taking niacin.
New Data:
In the large HPS2-THRIVE study, over 25,000 patients at high risk for a heart attack who were taking either simvastatin or simvastatin/ezetimibe (Vytorin) were randomized to take on top of these drugs either a placebo or Tredaptive – a drug produced by Merck containing niacin and an “anti-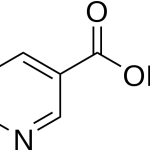 flushing agent” known as laropiprant. As expected, niacin caused average reductions in LDL of 10 mg/dl and triglycerides of 33 mg/dl while increasing HDL by 6 mg/dl, but provided no additional benefit over the statin alone in reducing the rate of heart attacks or other vascular events.
flushing agent” known as laropiprant. As expected, niacin caused average reductions in LDL of 10 mg/dl and triglycerides of 33 mg/dl while increasing HDL by 6 mg/dl, but provided no additional benefit over the statin alone in reducing the rate of heart attacks or other vascular events.
Making matter worse, the Tredaptive group experienced a high rate serious adverse events, i.e., every 3 out of 100 niacin-treated patients suffered from increased bleeding, infections, new onset diabetes, or other serious side effect. However, since these side effects had not been seen in other niacin+statin trials, it is extremely likely the side effects were due to the anti-flushing agent. Consistent with other combination trials, the use of niacin with a statin increased the likelihood of muscle damage caused by the statin.
Commentary:
This trial made absolutely no sense to conduct as the average LDL in the group was 63 mg/dl – well below the recommended level of less than 100 mg/dl for this patient population. Even in high risk individuals it would be highly unlikely that further reduction of LDL would show any significant impact on reducing cardiovascular mortality.
The conventional medical community is having a field day commenting on this study. There are many misleading statements being made in the press. This study does not erase the considerable scientific base of niacin as a medicine. It only casts a blow in using niacin with an anti-flushing taking statin drugs who have well-controlled LDL levels.
While niacin is definitely effective on its own and offers a viable alternative to statins, I do agree with the HPS2-THRIVE finding that niacin should not be used in high-risk patients with low LDL levels.
What has yet to be determined is the effect of niacin combined with a statin in patients with poorly controlled LDL and low HDL. That is the study that needs to be performed.
Reference:
Armitage J, et al .HPS2-THRIVE: Randomized placebo-controlled trial of ER niacin and laropriprant in 25,673 patients with pre-existing cardiovascular disease” ACC 2013. See also: http://www.thrivestudy.org/press_release.htm


